Rx for Health Care: A Doctor’s Perspective on the Past, Present and Future
This article was originally published on the Well Connected Twin Cities website March 15, 2019.
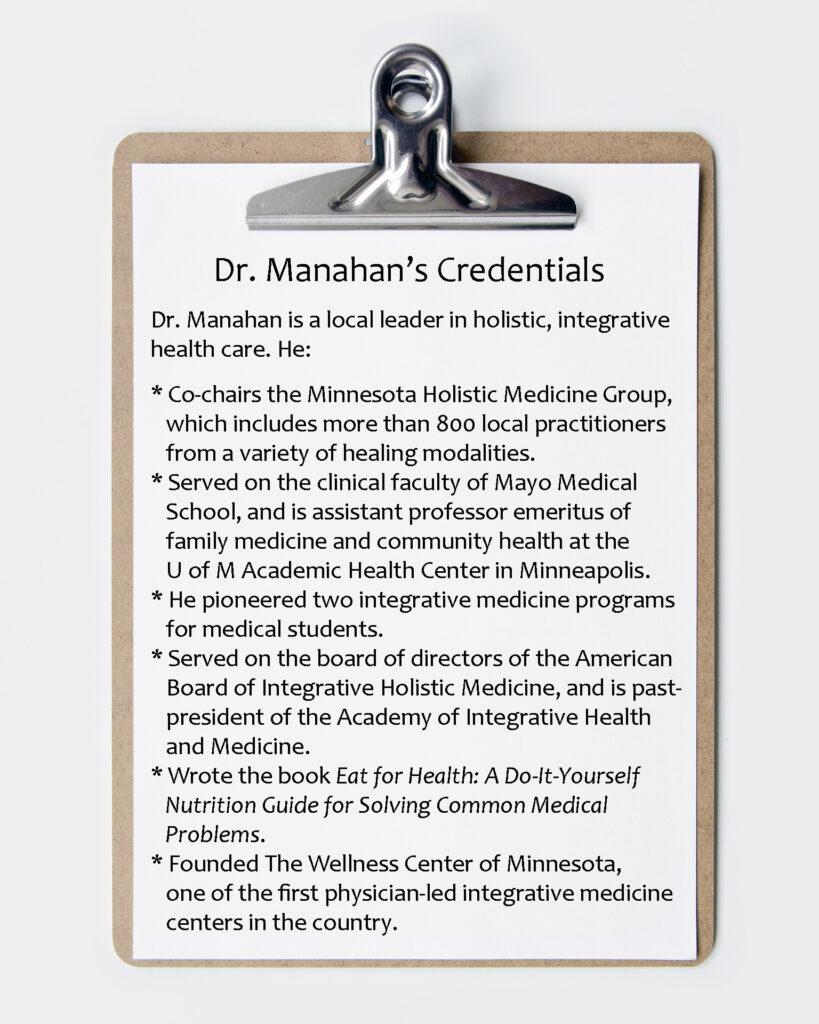
Bill Manahan, MD, has been part of the medical field for 50 years. He was an early advocate of integrative medicine, and is still nudging the medical field to embrace a more holistic approach to caring for patients.
While health care needs have changed dramatically, the health care system has been slow to adapt. As a result, a growing number of patients are seeking alternative options and many practitioners have started their own cash-based practices, free from insurance requirements so they can focus sufficient time and efforts on helping patients achieve wellness. Dr. Manahan believes conventional medicine would do well to learn from their approach to patient care.
Changes in Health Care Needs – 1960s to Today
“In the ‘70s, probably 75 percent of patients who came into my office had acute medical problems such as cuts, fractures, or illnesses like pneumonia or bronchitis,” says Dr. Manahan. “When I left practice 30 years later, probably 80 percent of my patients had chronic problems.”
In the 1960-70s, he explains, there was no need to address lifestyle choices like diet or exercise because medical needs were easily solved with singular treatments like stitches, antibiotics or surgeries. Patients went to their doctors with problems, and the doctors fixed the problems.

From the 1960s to today, the population has aged significantly and experienced major changes in diet, exercise, stress, environment and social connections, which have impacted health. Dr. Manahan points out that while advancements improve the quality of life, they also have drawbacks, including health implications. A few examples:
- Lead pipes deliver treated water to homes, but lead causes health issues when it leaches into the water.
- Fast and processed food reduces the time needed to prepare meals, but the chemicals, sugar and bioengineered ingredients aren’t healthy.
- New houses are more energy efficient, but can lead to mold and poor indoor air quality if they’re too tight.
As our society has advanced, so have complex and chronic medical issues caused by multiple lifestyle and environmental factors. Conditions like rheumatoid arthritis, osteoporosis, depression, cancer, type 2 diabetes, chronic pain, and chronic fatigue usually have multiple causes and involve multiple organ systems.

Because of the nature of chronic illnesses, the roles of physicians and patients have changed. Doctors can no longer solve patients’ problems with simple solutions. A whole systems, patient-centered, lifestyle approach is now required for good health care, explains Dr. Manahan. Often, patients need to take an active role in their treatments by making lifestyle changes.
Changes in the Health Care System?
While conventional medicine excels at emergencies and acute care, it needs improvement in addressing chronic care.
Both patients and physicians are frustrated with office visits that are too short to get to the cause of the problem, the lack of understanding about the role lifestyle plays, and the inability of prescription medication to resolve complicated health issues.
“That’s one reason there’s so much burnout in practitioners and why patients are so dissatisfied with out-patient medicine, because we’re still basically using the same system in 2019 that we used in the 1970s,” says Dr. Manahan. “Doctors still see patients for 15-20 minutes, which works for acute problems, but makes no sense for chronic problems … It’s truly like putting a bandaid over a gushing wound, the way we’re practicing out-patient medicine now.”
Integrative, Holistic Health Care
Dr. Manahan has met many people who have worked with integrative, holistic practitioners and made remarkable recoveries from problems conventional medicine was not able to resolve. He says:
“I feel both elation that these patients are doing so much better and sadness that so many others with similar conditions are suffering needlessly. Adequate knowledge and appropriate treatments are available to significantly help a majority of people suffering from chronic medical problems, but the cultural shift of these tests and treatments being acceptable for all physicians has not yet occurred. Therefore, these treatments are not yet easily available to most people.”
Wanting to learn how patient visits with holistic practitioners differs from conventional physicians, Dr. Manahan shadowed 20 integrative practitioners. The result was his vision for the future of health care, which he calls the “Whole Systems Medicine of Tomorrow.”

Vision for the Future of Health Care
Dr. Manahan’s vision for the Whole Systems Medicine of Tomorrow includes:
- Patient-Centered Care – The person, not the diagnosis or disease, is the target of treatment.
- Teamwork – The patient and practitioner work together on an appropriate course of action.
- Time – The practitioner takes the time to hear the patient’s story, take a good history and answer questions.
- Root Cause – Practitioners and patients work hard to discover the story behind and the root cause of the diagnosis. For example, asthma may be due to a moldy rug in the bedroom or a need to express oneself. Irritable bowel issues may indicate gluten, dairy or other foods are not in the patient’s best interest. Severe headaches may relate to job or relationship problems, musculoskeletal problems, certain offending foods, or a combination of factors.
- Holistic View – Practitioners take the time to evaluate mind, body, spirit, social and environmental factors that might contribute to patients’ problems.
- Lifestyle Factors – Healthy lifestyle choices are taken seriously; nutrition, gut health, exercise, sleep, and stress reduction are important factors in health.
- Uniqueness – Practitioners recognize each patient, and his/her biochemistry, is unique. Successful treatments for the same illness can vary between patients.
- Integrative Approach – There is a healthy balance between using conventional medicine when it works best (and recognizing the limitations and side effects of prescription medicine), and leveraging other approaches when they work better.
- Collaboration – Many types of practitioners work together as a team with a variety of methodologies to help improve each patient’s health.
- Current – Physicians are informed of the latest research findings, and are willing to adapt their practices in the best interest of patients.
How to Get There
The medical and insurance systems are so big, powerful and intertwined that Dr. Manahan believes change will require a major catastrophe – or a groundswell of people demanding it.
He’s encouraged by the number of patients, particularly women, who want to get to the root causes of their problems. “Those people are changing health care, too. The patient is the leader.”